Filler Complications
Introduction
The increased popularity of dermal fillers in enhancing facial aesthetics is due to their minimally invasive nature, short recovery time, and excellent outcomes. While collagen fillers dominated the market for over 20 years since their approval by the Food and Drug Administration (FDA) in 1981, it was the emergence of hyaluronic acid (HA) fillers that paved the way for new filler brands and technologies.
As with any medical procedure, a multitude of complications can occur after filler injection. The supposed reversibility of HA-based fillers adds their popularity; however, increased use of these fillers also puts less common but significant side effects in the spotlight. Injecting physicians must be aware of the adverse effects associated with dermal fillers because some of these complications can be devastating and irreversible. Additionally, some complications occur more frequently with specific filler materials or products; thus, the injector must know the properties of each filler at their disposal.
Patient Evaluation
As many complications are due to problems with injection technique, it is important to train extensively and gain experience, preferably with a reversible filler, in order to minimize potential problems. However, side effects are also related to the inherent properties of the filler or unappreciated patient factors.1 Patients presenting with complications after a filler injection should be questioned about previous medical procedures, filler-related issues, number of injections and treated areas.2 Immunosuppressed patients must be counseled for higher risk of infection. In patients with immunologic diseases, it is recommended to consult the rheumatologist or dermatologist before performing additional procedures.
If a patient is not satisfied with previous filler outcomes, the physician should not re-administer the same product. It is best to suggest an alternative filler material or treatment modality, or not treat at all. In attempting to remedy a complication, the patient should be informed that the elective treatment might require multiple sessions. It is also important to inform the patient that such interventions may result to permanent scarring.
Pre-Procedure Considerations
The best way to treat complications is to prevent them from occurring. Providing excellent predictable outcomes and avoiding unsatisfactory results begins before the actual injection process. While there is no filler product available without concomitant side effects, the physician can minimize complications by choosing the appropriate filler type and injection technique. Not all hyaluronic acid fillers have the same properties and indications. Each filler differs in cohesiveness, molecular size, and cross-linking technologies. In patients who have been treated multiple times, a detailed facial surgery and filler history should be obtained to guide the decision to inject, the placement of the product, and the type of filler to use.
The patients’ expectations should be managed. Completing a proper initial evaluation prior to injection is essential. The priority of the treatment is to satisfy the patient, thus before and after photographs should be taken. During the initial assessment, identify asymmetries and discuss each skin concern to facilitate a clear and honest discussion towards achieving the patient’s desired outcome. It is also essential to discuss the financial commitment involved in pursuing the treatment plan, including the number of syringes needed and if subsequent sessions will be necessary to reach the patient’s intended goal.
Skin Testing
The reactivity profile of the chosen filler should be reviewed prior to injection. Any filling material from foreign sources can theoretically trigger immune reactions to a variable degree, from redness to anaphylaxis. Products that are highly reactive, such as those containing bovine collagen, require skin testing prior to injection.3 Anaphylaxis is extremely rare but the Food and Drug Administration (FDA) still requires allergy testing for these products. The most popular filler material, hyaluronic acid, has a low rate of hypersensitivity, ranging from 0.6% to 0.8% regardless if the formula is bacterial or viral in origin.4 Hypersensitivity reactions to bovine collagen may be local or systemic while reported reactions to hyaluronic acid were often immediate, localized, and typically resolved within three weeks.5
The use of collagen fillers has declined due to the development of new fillers with better safety profiles. New products containing hyaluronic acid and calcium hydroxyapatite have been found to be superior to collagen with a very small chance of local reactions. Popular bovine collagen and human collagen products are no longer being manufactured; the only product available with 80% purified bovine collagen, which requires skin testing, has polymethylmethacrylate as the main ingredient (Artefill).
Filler Selection
Product-related complications are influenced by the physiochemical properties of the filler and the patient’s response to the product.6 Currently, available fillers may be classified as temporary or permanent. Temporary fillers are biodegradable and are absorbed or metabolized by the body. The duration of effects of these fillers vary and is dependent on the type and amount of filler injected, treatment location, and injection technique utilized.7 Temporary fillers cleared by the FDA include hyaluronic acid, collagen, calcium hydroxylapatite (CaHA), and poly-l-lactic acid (PLLA). The only FDA-approved permanent filler contains biocompatible, non-biodegradable polymethylmethacrylate (PMMA) beads intended to reduce wrinkles around the mouth, and recently, for the treatment of acne scars.
Inappropriate Placement and Its Manifestations
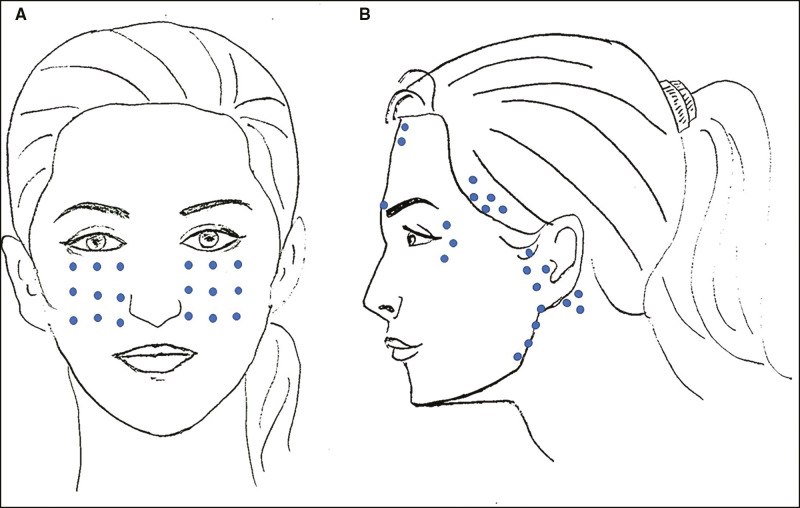
It is imperative to understand the underlying body, soft tissue structures and vascular anatomy when injecting facial fillers. Accurate and safe placement of filler products depends not only on these factors but also on thorough understanding of the patient’s history and the product’s properties. Inappropriate placement of fillers, such as superficial injection, can lead to a range of complications. Injecting too superficially is a common error and may result in inflammatory nodule formation, visible product, a bluish hue under the skin, and hypertrophic scarring.8,9 While these reactions can be somewhat prevented by the use of correct injection technique, they can, however, cause anxiety and dissatisfaction for patients.
Simple lumps and bumps associated with superficial placement can be alleviated by massaging the area, as well as through aspiration or incision and drainage.10 If the reaction is due to an hyaluronic acid product, hyaluronidase can help treat this problem. Polymethylmethacrylate plus collagen is a permanent filler that, less forgiving, can be associated with another set of complications such as long-lasting itching and redness. If the product in question contains calcium hydroxyapatite (Radiesse), superficial injection is associated with white nodule formation. This is often managed by puncturing and expressing the nodules using a No 11 blade or needle.11 The same technique is used if the injecting physician overfills a particular area. Massaging the area to disperse the product is an adequate solution in some cases; however, one can puncture the skin and express excess filler if the overfill persists.
Injection Site Reactions
Despite best practices, including allergic testing and proper product selection, reactions can still occur. Local injection site reactions are the most common side effect associated with filler injection since it requires skin piercing and introduction of a foreign substance. Other foreign materials other than the filler, such as residual makeup incompletely removed from the patient’s skin, could cause a reaction; therefore, makeup in the injection area must be removed prior to application. The most commonly observed reactions are redness, swelling, bruising, tenderness or pain, and itchiness. These reactions are often mild to moderate and could last for a few days to a week.
Edema and ecchymosis are often due to injection technique, speed of injection, and filler choice. Regardless of the product injected, swelling and bruising are usually localized, mild, and self-limiting. Comparing the package inserts of some popular fillers: Juvederm Ultra (HA) has an 86% reported incidence of swelling and 59% incidence of bruising; Injections from Sculptra (PLLA) has 4-7% incidence of swelling and 6-38% incidence of bruising; and the use of Radiesse treatment (CaHA) has a reported 69.2% incidence of swelling and 63.2% incidence of bruising.12,13,14 Dr. John Quinn suggests using the smallest needle possible and microcannula for danger areas to reduce the risk of swelling and bruising. This is particularly important when augmenting the lip as the labial artery runs deep in the body of the lips, thus the border between wet and dry area is more likely to bruise.
Early Onset Complications
One of the most devastating complications of soft tissue augmentation with injectables is intravascular injection, which can lead to potential tissue necrosis, scarring, and even blindness. The best treatment for vascular compromise begins with sufficient prevention. Thorough knowledge of facial anatomy and awareness of danger zones reduces the risk, but actual vascular structures possess considerable variation. Early recognition of the warning signs is highly important as the injecting physician must be ready to administer appropriate treatment immediately. Hyaluronidase and other supplemental treatments, such as a warm compress, nitro paste, and sildenafil, must be immediately available.
The glabella, nasolabial fold, and nose are the most common danger zones, as these areas have rich anastomoses with the internal carotid artery.15 Nose reshaping with facial fillers has become a common procedure in the past few years. Because of the increasing incidence of nasal tip necrosis due to the compression of facial blood vessels in the area, this procedure should be performed by specialists rather than newly trained practitioners. Post-injection blindness is not a commonly reported side effect with dermal filler, but knowing proper management and prevention is paramount. Pain and pallor are common signs of arterial compromise. Embolization and compression of the glabellar arteries can occur due to the small amount of space between the skin and periosteum in this area.8 In the event of a vascular compromise, treatment includes massage, hyaluronidase, heat, and topical GTN.
Delayed Onset Complications
Delayed onset nodule formation and granulomatous reactions have been reported with several filler products. Biofilms may play a role in the presentation of delayed onset erythematous nodules (“angry red bumps”). These bumps are different from ordinary nodules (collections of injected fillers) and are regarded as possible foreign body reactions, hypersensitivity reactions, infections, or sterile abscesses. To help minimize the risk of infection, clean preparation of the skin using chlorhexidine is recommended prior to filler injection. A granuloma is an immune response to an implanted foreign material and develops via an accumulation of immune-related cells, such as lymphocytes, in an attempt to eliminate the foreign body.16
In contrast to granuloma, the key signs of infection are erythema, warmth, and tenderness. The usual cause of late onset infection is less common bacteria like mycobacteria.17 Successful treatment requires appropriate antibiotic therapy as well as aggressive debridement of all infected skin and subcutaneous tissue. Dr. Quinn prescribes clarithromycin 500 mg twice a day for four weeks, while other physicians advise the use of ciprofloxacin 750 mg bd for a month.
Implanted fillers can migrate up to several years after injection. Semi-permanent and permanent fillers are most likely to migrate, but infection or delayed granuloma can also trigger migration. If the injected product is HA-based, hyaluronidase is the preferred treatment, but surgical removal may be necessary for other filler materials.
Conclusion
Being an efficient alternative to enhance facial aesthetics with downtime at a minimum, dermal fillers are the gold standard-bearer for soft-tissue augmentation. While adverse events certainly are rare, practicing caution during injection, alongside public education on the potentially catastrophic consequences to health, of unregulated filler injection are essential. It is the responsibility of the physician to consider the individual characteristics of each patients and the properties of available fillers when selecting a treatment. The physician’s readiness to handle various adverse events, and careful following of treatment consensus in the occurrence of a nodule, granuloma, or vascular compromise, ensures optimal management.
References
1. Leonhardt, J.M., Lawrence, N., & Narins, R.S. Angioedema acute hypersensitivity reaction to injectable hyaluronic acid, Dermatol Surg, 31, 5.
2.Jin Moon, H., & Sook Yi J. (2016). Management of Facial Filler InjectionComplications in Aesthetic Plastic Surgery of the East Asian Face, Thieme, p. 406
3. Bailey, S., Cohen, J., & Kenkel, J. (2011). Etiology, Prevention, and Treatment of Dermal Filler Complications, Aesthetic Surgery Journal, 31, 1.
4. Andre, P. (2004). Evaluation of the safety of a non-animal stabilized hyaluronic acid (NASHA—Q-Medical, Sweden) in European countries: a retrospective study from 1997 to 2001, J Eur Acad Dermatol Venereol, 18, 4.
5. Friedman, P.M., Mafong, E.A., Kauvar, A.N., & Geronemus, R.G. (2002). Safety data of injectable nonanimal stabilized hyaluronic acid gel for soft tissue augmentation. Dermatol Surg, 28, 6.
6. Gravier, M., Bass, L., Lorence, P., et al. (2018). Differentiating non-permanent injectable fillers: Prevention and treatment of filler complications, Aesthetic Surgery Journal, 38, 1.
7. Luebberding, S., & Alexiades-Armenakas, M. (2013). Critical appraisal of the safety of dermal fillers: a primer for clinicians, Curr Derm Rep
8. Narins, R.S.M., Jewell, M.M., Rubin, M.M., Cohen, J.M., & Strobos, J.M. (2006). Clinical conference: management of rare events following dermal fillers-focal necrosis and angry red bumps, Dermatol Surg, 32.
9. Zielke, H., Wölber, L., Wiest, L., Rzany, B. (2008). Risk profiles of different injectable fillers: results from the injectable filler safety study (IFS Study), Dermatol Surg, 35, 1.
10. Brody, H.J. (2005). Use of hyaluronidase in the treatment of granulomatous hyaluronic acid reactions or unwanted hyaluronic acid misplacement, Dermatol Surg, 34, 1.
11. Berlin, A., Cohen, J.L., & Goldberg, D.J. (2006). Calcium hydroxylapatite for facial rejuvenation, Semin Cutan Med Surg, 25.
12. Juvederm package insert. [Available from: http://www3.juvederm.com/professionals/pdf/juvederm_dfu.pdf ]. Accessed April 1, 2019.
13. Sculptra package insert. [Available from: http://products.sanofi -aventis.us/sculptra/sculptra.html ]. Accessed April 1, 2019.
14. Radiesse Injectable Implant Instructions For Use. [Available from: http://www.accessdata.fda.gov/cdrh_docs/pdf5/P050037c.pdf ]. Accessed April 1, 2019.
15. Brennan, C. (2014). Avoiding the “danger zones” when injecting dermal fillers and volume enhancers, Plast Surg Nurs, 34, 3.
16. Sidwell, R.U., Dhillon, A.P., Butler, P.E., & Rustin, M.H. (2004). Localized granulomatous reaction to a semi-permanent hyaluronic acid and acrylic hydrogel cosmetic filler, Clin Exp Dermatol, 29.
17. Hirsch, R.J., Narurkar, V., & Carruthers, J. (2006). Management of injected hyaluronic acid induced Tyndall effects, Lasers SurgMed, 33, 3.
18. Plaus, W.J., & Hermann, G. (1991). The surgical management of superficial infections caused by atypical mycobacteria, Surgery, 110.