Dermal fillers are now among the most common aesthetic procedures worldwide. When performed correctly, they are safe and effective, but serious complications can still occur.
The most critical of these is vascular occlusion (VO) — an interruption of blood flow caused by filler entering or compressing a vessel. VO can rapidly lead to tissue ischemia, necrosis, or even blindness.
Although rare, its consequences can be severe. Outcomes often depend on how quickly the event is recognized and treated. Early identification and prompt use of hyaluronidase can restore perfusion and prevent long-term damage.
Recent guidelines, including the Complications in Medical Aesthetics Collaborative (CMAC) recommendations, provide structured protocols for recognizing, staging, and managing VO. This article summarizes current evidence and best practices to help aesthetic practitioners prevent, identify, and treat vascular occlusion swiftly and effectively.
Understanding Vascular Occlusion
A vascular occlusion (VO) occurs when blood flow is disrupted.
This can happen one of two ways:
- Intravascular injection – the filler directly enters an artery or vein.
- Extrinsic compression – the filler bolus or edema externally compresses a vessel.
Both can lead to tissue ischemia if circulation is not promptly restored.
Not all vascular occlusions are the same. The risk depends on anatomy, product characteristics, and injection technique.
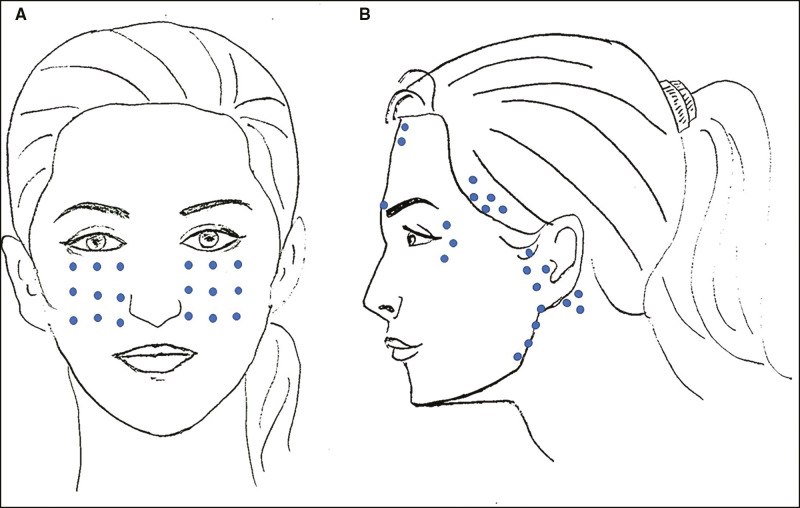
High-Risk Anatomical Areas
The following regions contain terminal arterial branches and have limited collateral supply:
- Glabella
- Nasal dorsum
- Nasolabial folds
- Lips
- Temple
Any blockage here can quickly compromise perfusion. (King et al., 2020)
Filler Rheology and Technique
Products with high elasticity (G’) and viscosity can exert greater pressure on vessels or form more stable emboli.
High-risk techniques include:
- Needle injections
- Deep boluses
- High-pressure delivery
Lower-risk approaches include slow, low-volume, linear threading with a cannula — though even cannulas are not completely protective. (Aesthetic Plast Surg 2025)
Patient-Specific Factors
- Prior filler placement – may distort anatomy or compress vessels, leaving less space for new product.
- Vascular disease – reduces vessel elasticity and impairs circulation.
- Post-surgical scarring – alters normal vascular pathways and can trap filler near fragile vessels.
Understanding facial angiosomes—the vascular territories supplied by specific arteries—helps practitioners predict where ischemia may appear and guides safer technique.
Recognizing the Signs and Symptoms
Early recognition of VO is essential. The faster it’s identified, the greater the chance of reversing ischemia and preventing necrosis or vision loss.
There are four main stages where signs can appear: during injection, shortly after injection, several hours later, or as an ocular emergency.
During Injection
Watch for:
- Sudden blanching or whitening of the skin
- Sharp, severe pain out of proportion to the injection
- Resistance or back-pressure on the plunger
- Livedo or mottled discoloration within seconds
These symptoms suggest intravascular filler placement or arterial compression.
Early Post-Injection (Minutes to Hours)
Signs may develop gradually:
- Dusky or bluish skin tone
- Prolonged capillary refill (> 2 s)
- Cool or pale skin
- Reticulated erythema
- Increasing pain
Treat any of these findings as ischemia until proven otherwise. (CMAC Guideline 2022)
Late Signs (Hours to Days)
- Pustules within 24–72 h
- Gray or black necrosis
- Crusting or ulceration
These indicate established tissue death and require wound care and possible debridement.
Ocular or Neurologic Warning Signs
This represents an emergency.
If the patient experiences:
- Sudden vision loss or blurriness
- Double vision
- Eye pain, headache, or dizziness
- Drooping eyelid or limited eye movement
Immediately stop, keep the patient upright, and contact an ophthalmologist. These findings suggest retrograde embolization into the ophthalmic artery — intervention within minutes can preserve vision. (Beleznay et al., 2015, Aesthet Surg J.)
Immediate Management Protocol
When VO is suspected, intervention must begin at once. The objective is to restore blood flow before ischemia becomes irreversible.
The first action is to stop injecting immediately. Keep the needle or cannula in place to guide possible hyaluronidase delivery. Avoid massaging the area until evaluation is complete.
Next, assess and document:
- Blanching, livedo, or pain
- Capillary refill time (> 2 s)
- Skin temperature and color changes
Outline the affected zone and photograph for monitoring.
If a hyaluronic acid filler was used, proceed with hyaluronidase:
- High-dose, pulsed injections (≈ 1500 IU) into and around the ischemic area
- Multiple small injections across the region (the “flooding technique”)
- Repeat every 15–20 minutes until perfusion improves
Adjunctive measures can enhance recovery:
- Warm compresses for vasodilation
- Gentle massage after hyaluronidase
- Aspirin 300 mg for antiplatelet effect
- Topical nitroglycerin (short-term vasodilation)
- Corticosteroids to limit inflammation
- Hyperbaric oxygen therapy (HBOT) for delayed or severe ischemia (Cox et al., 2021, Dermatol Surg.)
If visual symptoms appear, treat as a true emergency — contact ophthalmology immediately, keep the patient upright, and arrange hospital transfer without delay.
Document all steps taken, noting times, dosages, and patient response. Continue monitoring every 30–60 minutes until normal skin perfusion returns.
Post-Event Care and Follow-Up
Once blood flow is restored, focus shifts to healing and secondary prevention.
Observe the treated area for several hours, checking for color change, pain, or new discoloration. Persistent or worsening symptoms may indicate incomplete reperfusion.
If necrosis develops, manage the wound carefully:
- Gentle cleansing and non-adherent dressings
- Topical or oral antibiotics if infection risk is present
- Adequate pain control and patient reassurance
For extensive ischemia, HBOT can improve oxygen delivery and promote recovery. Pentoxifylline or low-molecular-weight heparin may support microcirculation, though evidence is limited.
Patients should be reviewed daily until stable, then weekly until healed.
Documentation with serial photos supports both medical follow-up and medicolegal transparency.
Psychological care matters too. Compassionate communication and consistent follow-up help maintain patient trust after a stressful event.
Prevention Strategies
The best management is prevention. While VO cannot be eliminated entirely, risk can be dramatically reduced through preparation, anatomical awareness, and cautious technique.
Begin every session with a risk assessment:
- Review prior filler treatments
- Assess vascular health
- Note any surgical scarring or trauma
Anatomical knowledge is essential.
High-risk areas include:
- Glabella
- Nose
- Nasolabial folds
- Lips
- Temple
Use safer techniques:
- Inject slowly and with minimal pressure
- Use small aliquots
- Keep the needle in motion
- Aspirate before injection (though not fully reliable)
- Consider a blunt cannula in high-risk zones
Select hyaluronic acid fillers when possible in critical regions, since they are reversible. Avoid unnecessary filler layering or excessive volume.
Every clinic should keep a vascular occlusion emergency kit stocked with:
- Hyaluronidase (multiple vials)
- Aspirin
- Topical nitroglycerin
- Sterile syringes and needles
- Contact details for ophthalmology and HBOT centers
Educate every patient about red-flag symptoms and provide after-hours contact details.
Continuous training, simulation drills, and case reviews ensure the entire team is prepared for rapid, coordinated action.
Conclusion
Vascular occlusion is the most serious but also the most preventable complication in dermal filler practice.
Preparedness, anatomical mastery, and calm execution of protocol are the cornerstones of safety.
When occlusion occurs, speed and structure save tissue—and sometimes vision.
Each event offers a chance to refine skill, reinforce vigilance, and strengthen clinical systems.
The safest injector is not the one who never faces complications,
but the one who recognizes them early, acts decisively, and never stops learning.
References
- Complications in Medical Aesthetics Collaborative (CMAC) Guideline for Hyaluronic Acid Vascular Occlusion, 2022. Journal of Clinical and Aesthetic Dermatology.
- King M, et al. Management of Hyaluronic Acid Filler-Induced Vascular Occlusion: A Review. Aesthetic Surgery Journal. 2020. PMCID: PMC7028373
- Beleznay K, et al. Avoiding and Treating Blindness From Fillers: A Review of the World Literature. Aesthetic Surgery Journal. 2015. PubMed: 26182000
- Cox S, et al. Adjunctive Hyperbaric Oxygen for Filler-Induced Ischemia: Evidence and Practical Application. Dermatologic Surgery. 2021. PubMed: 34098754
- Aesthetic Plastic Surgery (2025). FOEM2 Classification of Filler-Induced Cutaneous Ischemia. SpringerLink
National Center for Biotechnology Information (NCBI). Hyaluronidase: Mechanism and Clinical Use. NBK554607