
Top 10 Male Plastic Surgery Trends in 2026
Male plastic surgery is no longer a small niche within aesthetic care.

2026 Conference Insights: The Biggest Innovations Announced at IMCAS & AMWC
Two major congresses are setting the tone for 2026 in aesthetic medicine: IMCAS World Congress 2026 (Paris + online, Jan 29–31, 2026) and AMWC Monaco 2026 (Mar 26–28, 2026).
What’s most interesting isn’t a single “breakthrough product,” but a clear, shared direction: regeneration, skin quality, smarter planning (AI), safer practice, and combination protocols—all framed as practical, clinic-ready upgrades.
AI in Aesthetic Medicine
AI in aesthetic medicine is redefining how clinicians assess faces, plan treatments, and predict outcomes with a level of precision that was previously unattainable through visual analysis alone.
Recognizing and Managing Vascular Occlusion After Dermal Fillers
Dermal fillers are now among the most common aesthetic procedures worldwide.
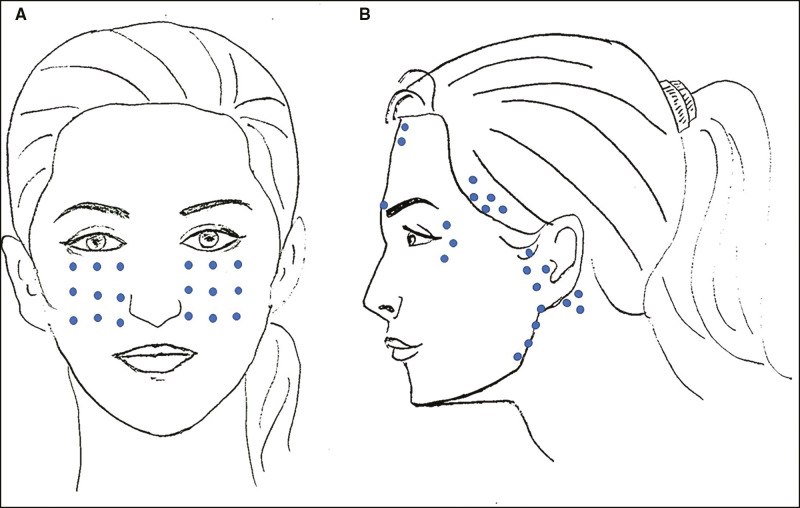
Botox Microdroplet Technique — Everything You Need to Know
Botox microdroplet injections use botulinum toxin type A to smooth out the skin, improve texture, and reduce shine.

Role of Biostimulators in Facial Rejuvenaton
As aesthetic practitioners seek more natural and long-lasting solutions for patients, the use of biostimulators injections has risen substantially.

HIPAA for Dermatologists: Guide to Staying Compliant
Running a dermatology practice requires a constant clinical focus on patient care—diagnosing, managing, and treating skin conditions—making it easy for administrative priorities like the Health Insurance Portability and Accountability Act of 1996 (HIPAA) regulation to fall to the bottom of the to-do list.

How to Deal with an Angry Patient
Managing an angry patient is an inevitable part of a healthcare provider’s life.

Dermatologist Marketing Ideas to Grow Your Practice
As a dermatologist, your expertise brings relief and hope to patients battling various skin conditions.

Polynucleotides Under Eyes: Benefits, Side Effects, Injection Technique, and More
Polynucleotides under eyes are a promising regenerative solution for addressing age-related periorbital issues.

Do’s and Don’t of Chemical Peels for Sensitive Skin
There is a misconception about using sensitive skin chemical peels, as they are said to be already harsh on any skin type, even that of the best condition.

Expert Guide for Medical Device Inventory Management
Effective medical device inventory management is crucial for healthcare facilities to ensure the availability, safety, and proper functioning of medical equipment.