AI in aesthetic medicine is redefining how clinicians assess faces, plan treatments, and predict outcomes with a level of precision that was previously unattainable through visual analysis alone. As aesthetic medicine becomes more data-driven, artificial intelligence is shifting clinical decision-making away from intuition toward quantifiable risk modeling, anatomical mapping, and outcome simulation. This transformation is not theoretical—AI systems are already being used to analyze facial symmetry, assess skin quality, predict aging patterns, and support injection planning with algorithmic accuracy.
Rather than replacing medical judgment, AI functions as an advanced diagnostic extension of the clinician. Through artificial intelligence in dermatology, practitioners gain objective insight into skin structure, vascular patterns, and tissue quality, allowing for more precise product selection and depth planning. Technologies such as facial analysis software for injectors and AI skin assessment technology provide reproducible measurements where visual estimation once dominated. The result is greater treatment consistency, improved patient communication, and more controlled clinical outcomes.
From early diagnostics to dynamic simulations and procedure support, AI is becoming embedded within aesthetic workflows. The most successful clinics will not be those that adopt technology indiscriminately, but those that integrate intelligence strategically—using algorithms to assist, validate, and refine human expertise.
Key Takeaways
- AI in aesthetic medicine enhances accuracy in diagnostics, planning, and execution
- Algorithms support objective skin and facial assessments
- AI improves outcome predictability and patient communication
- Digital analysis reduces operator variability
- Machine intelligence strengthens safety in injectable treatments
- Predictive modeling enables individualized protocols
- Technology complements—not replaces—clinical expertise
AI in Aesthetic Diagnostics and Skin Assessment
Artificial intelligence is bringing objectivity to one of the most subjective components of aesthetic medicine: skin evaluation. Through artificial intelligence in dermatology and advanced AI skin assessment technology, clinicians can now quantify variables such as dermal thickness, hydration, pigmentation, vascular activity, and textural irregularities with consistency that exceeds human visual capability.
These systems use multispectral imaging, pattern recognition, and machine learning to detect subtle features that may not be clinically visible, including early-stage dyschromia, inflammatory activity, and volume loss patterns.
Instead of relying on interpretation alone, practitioners now work with numerical benchmarks and progression analytics, allowing treatments to be guided by measurable data rather than assumption. This shift is especially relevant in complex injectable planning, where surface quality directly affects how product placement translates visually. AI also improves baseline documentation and follow-up by generating standardized reports that reduce variability between practitioners and allow longitudinal monitoring of tissue changes. The result is a more controlled diagnostic environment where decisions are supported by real metrics rather than observational bias.
- Quantification of skin quality parameters
- Automated wrinkle, pore, and redness analysis
- Objective pigment and vascular mapping
- Baseline documentation and progress tracking
- Enhanced diagnosis of inflammation and aging patterns
- Clinical risk stratification based on tissue condition
- Reduced inter-practitioner diagnostic variability
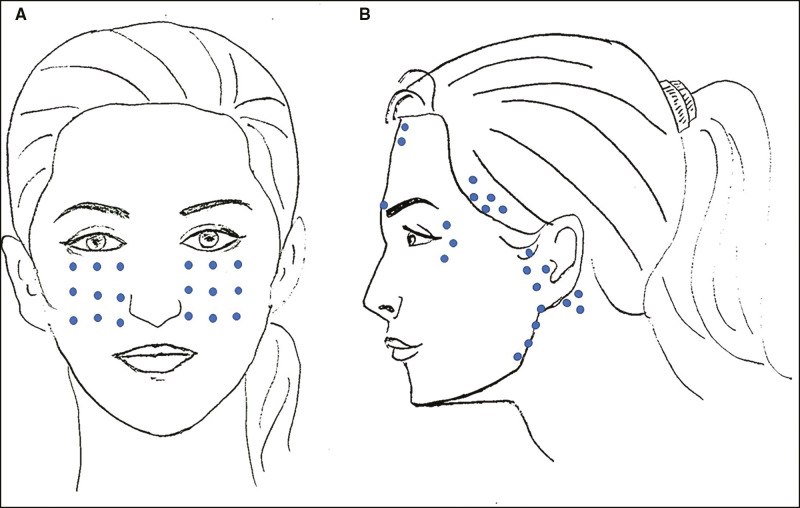
Facial Analysis and Treatment Planning with AI
Facial aesthetics is increasingly shaped by anatomy-driven design rather than artistic interpretation alone. Modern facial analysis software for injectors allows clinicians to evaluate symmetry, proportion, and volume distribution using algorithmic modeling that maps skeletal structure, fat compartments, and surface topography simultaneously.
Through digital tools for facial contouring, providers gain insight into facial dynamics across multiple vectors, predicting how aging, gravity, and product placement interact over time.
These systems analyze facial planes, angles, and proportions in real time, supporting treatment planning decisions that previously relied on experience alone. AI algorithms also support simulation modeling, enabling clinicians to preview projected outcomes before injecting. This improves patient communication and aligns expectations while allowing clinical decisions to be tested digitally before being applied physically.
Planning software does not eliminate creative control—it refines it by anchoring aesthetic judgment in anatomical reality. As a result, treatments shift from reactive volumization to proactive facial architecture design.
- Facial landmark detection and proportion analysis
- Automated symmetry and balance evaluation
- Predictive modeling of aging trajectories
- Simulation-based patient consultations
- Vector and depth planning assistance
- Treatment protocol standardization
- Objective comparison of pre- and post-treatment structures
AI-Guided Injection Techniques
Injection accuracy is no longer based solely on tactile skill and anatomical memory. With AI-driven injection mapping and computer-assisted filler placement, clinicians are beginning to operate with digital guidance that improves depth control, anatomical targeting, and procedural safety.
These systems combine facial imaging, landmark detection, and vascular mapping to generate individualized injection grids based on each patient’s structural anatomy rather than template-based protocols. Instead of estimating depth or vector by experience alone, the operator receives visual guidance that identifies risk zones, optimal entry points, and recommended injection planes in real time or during pre-procedural planning.
This fundamentally changes how consistency is achieved across practitioners and practices. AI environments also support protocol standardization, reducing outcome variability between clinicians with different technical backgrounds. Most importantly, safety is enhanced through algorithmic identification of danger zones, including high-risk vascular territories.
As adoption increases, this technology is expected to significantly reduce complications related to improper plane selection and inaccurate product placement. Rather than automating the injector, AI elevates the injector—structuring precision into every step of the treatment.
- Algorithmic injection grid generation
- Automated depth and plane modeling
- Vascular risk-zone visualization
- Injection site optimization
- Pre-procedure simulation tools
- Reduction in technical variability
- Improved safety in high-risk zones
Predictive Modeling in Aesthetic Outcomes
One of the most disruptive capabilities of AI lies in its power to forecast results before treatment begins. Through predictive aesthetic outcomes, clinicians can simulate how filler, neuromodulators, and energy-based treatments are likely to behave in individual faces. Using patient-specific data, machine learning models estimate tissue response, volume retention, skin adaptation, and symmetry evolution over time.
This allows practitioners to evaluate multiple treatment strategies digitally before selecting the safest and most effective option clinically. In the consultation setting, predictive modeling improves transparency by visually illustrating likely changes, reducing the mismatch between patient expectations and achievable results.
Instead of describing outcomes abstractly, physicians can demonstrate anticipated modifications in facial contour, volume distribution, and surface quality. AI projection tools also assist in long-term planning by estimating how treatments interact with aging processes such as fat descent, bone resorption, and collagen loss.
This opens the door to regenerative and preventative strategies rather than reactive corrections. Predictive analytics therefore move aesthetic medicine from improvement to planning—from correction to design.
- Outcome simulation modeling
- Long-term aging prediction
- Treatment comparison systems
- Objective before–after forecasting
- Improved patient communication
- Response variability mapping
- Reduced dissatisfaction and revisions
Smart Devices and AI Integration in Clinical Practice
The clinical future of aesthetics extends beyond software into hardware. The emergence of smart injector systems represents the convergence of mechanical precision and algorithmic guidance, where devices are designed not only to deliver product, but to interpret data during delivery. These systems integrate pressure sensors, dosage tracking, and flow control with digital analytics to reduce variability and improve safety.
Powered by machine learning in cosmetic procedures, smart injectors learn from repeated use, optimizing injection speed, pressure, and depth in response to tissue resistance patterns. This type of feedback loop allows continuous improvement in technique across uses and users. Instead of relying on manual control alone, clinicians gain access to performance metrics that highlight inefficiencies, risks, and deviations from protocol.
Workflow is also optimized, as device software integrates with imaging platforms, patient records, and facial mapping tools. In time, AI devices may support automated alerts for high-risk injection zones or improper angle entry. These tools are not replacing clinician control; they are reinforcing it by delivering surgical-grade consistency in non-surgical procedures. As adoption expands, injector technology is likely to evolve rapidly from passive tool to active co-pilot.
- Real-time pressure and flow feedback
- Automated dosage tracking
- AI-assisted delivery optimization
- Safety alerts for anatomical risk zones
- Performance data collection
- Integration with treatment planning software
- Technique standardization across providers
Challenges, Ethics, and the Future Frontier
As AI accelerates in aesthetic medicine, its expansion introduces complex ethical, regulatory, and logistical challenges. Algorithms must be transparent, clinically validated, and continuously monitored. Bias within datasets can skew outcomes, particularly in patients with diverse skin types and facial structures. Clinical adoption therefore demands oversight, not blind faith. Data privacy also becomes a central concern as facial scans and biometric data are stored and analyzed at scale.
Physicians retain legal responsibility for outcomes regardless of software involvement, reinforcing the principle that AI is an aid—not an authority. Regulatory agencies are only beginning to establish parameters for diagnostic AI and procedural software in aesthetics, creating a temporary gap between innovation and oversight. Despite this, the trajectory is clear. Artificial intelligence will become embedded in nearly every stage of aesthetic workflows, from consultation to follow-up analysis.
The future will favor clinicians who develop both aesthetic judgment and technological literacy. Understanding what the machine does—and what it cannot—will be as essential as anatomy. Those who integrate AI strategically will increase efficiency without compromising safety. Those who rely on it blindly may inherit its limitations.
- Algorithm validation requirements
- Ethical limits of automation
- Data privacy and patient consent
- Liability considerations
- Regulatory uncertainty
- Bias in training datasets
- The evolving role of the physician
FAQ
1. How accurate is AI in aesthetic medicine for diagnosing skin conditions and facial asymmetry?
AI systems demonstrate high accuracy in pattern recognition, skin classification, and landmark detection when trained on validated datasets. In clinical use, AI enhances diagnostic precision but does not replace physician expertise. Final interpretation and treatment decisions remain the responsibility of the practitioner.
2. Can artificial intelligence replace clinical experience in aesthetic treatments?
No. AI is designed to support decision-making, not substitute clinical judgment. While algorithms improve consistency and data interpretation, aesthetic outcomes still depend on anatomical understanding, injection technique, and medical assessment.
3. Is AI-driven injection mapping approved for clinical use?
Some AI-assisted tools are cleared for use as clinical decision-support systems, while others remain under regulatory evaluation. Approval varies by jurisdiction and technology type. Physicians should ensure any solution used complies with FDA or CE regulations and local guidelines.
4. How reliable are predictive aesthetic outcomes generated by AI?
Predictive models estimate trends based on prior data, facial structure, and tissue characteristics. While useful for planning and communication, these projections reflect probability—not certainty—and must never be presented as guaranteed outcomes.
5. Does using AI in dermatology improve patient safety?
Yes, when implemented correctly. AI can identify vascular risk zones, support depth planning, and reduce technical variability—factors that significantly enhance procedural safety.
References (AMA style)
- Esteva A, Kuprel B, Novoa RA, et al. Dermatologist-level classification of skin cancer with deep neural networks. Nature. 2017;542(7639):115–118.
- Kalluri R, LeBleu VS. The biology, function, and biomedical applications of exosomes. Nat Rev Mol Cell Biol. 2020;21(3):142–156.
- Phinney DG, Pittenger MF. Concise review: MSC-derived exosomes for cell-free therapy. Stem Cells. 2017;35(4):851–858.
- Brinker TJ, Hekler A, Enk AH, et al. Deep neural networks are superior to dermatologists in melanoma image classification. Eur J Cancer. 2019;119:11–17.
- Tschandl P, Rinner C, Apalla Z, et al. Human–computer collaboration for skin cancer recognition. Nat Med. 2020;26(8):1229–1234.
Cotofana S, Sieber R, Schenck TL, et al. Facial danger zones for filler injections. Plast Reconstr Surg. 2015;135(6):1431–1439. - De Maio M, Swift A, Signorini M, Fagien S. Facial assessment and injection mapping. Plast Reconstr Surg. 2017;139(2):594–606.
- Bullock J, Alexandra L, Pham KH, et al. Mapping the landscape of artificial intelligence applications against COVID-19. J Med Internet Res. 2020;22(12):e21460.
- FDA. Artificial Intelligence and Machine Learning in Software as a Medical Device. U.S. Food and Drug Administration. 2021.
- Topol EJ. High-performance medicine: the convergence of human and artificial intelligence. Nat Med. 2019;25(1):44–56.