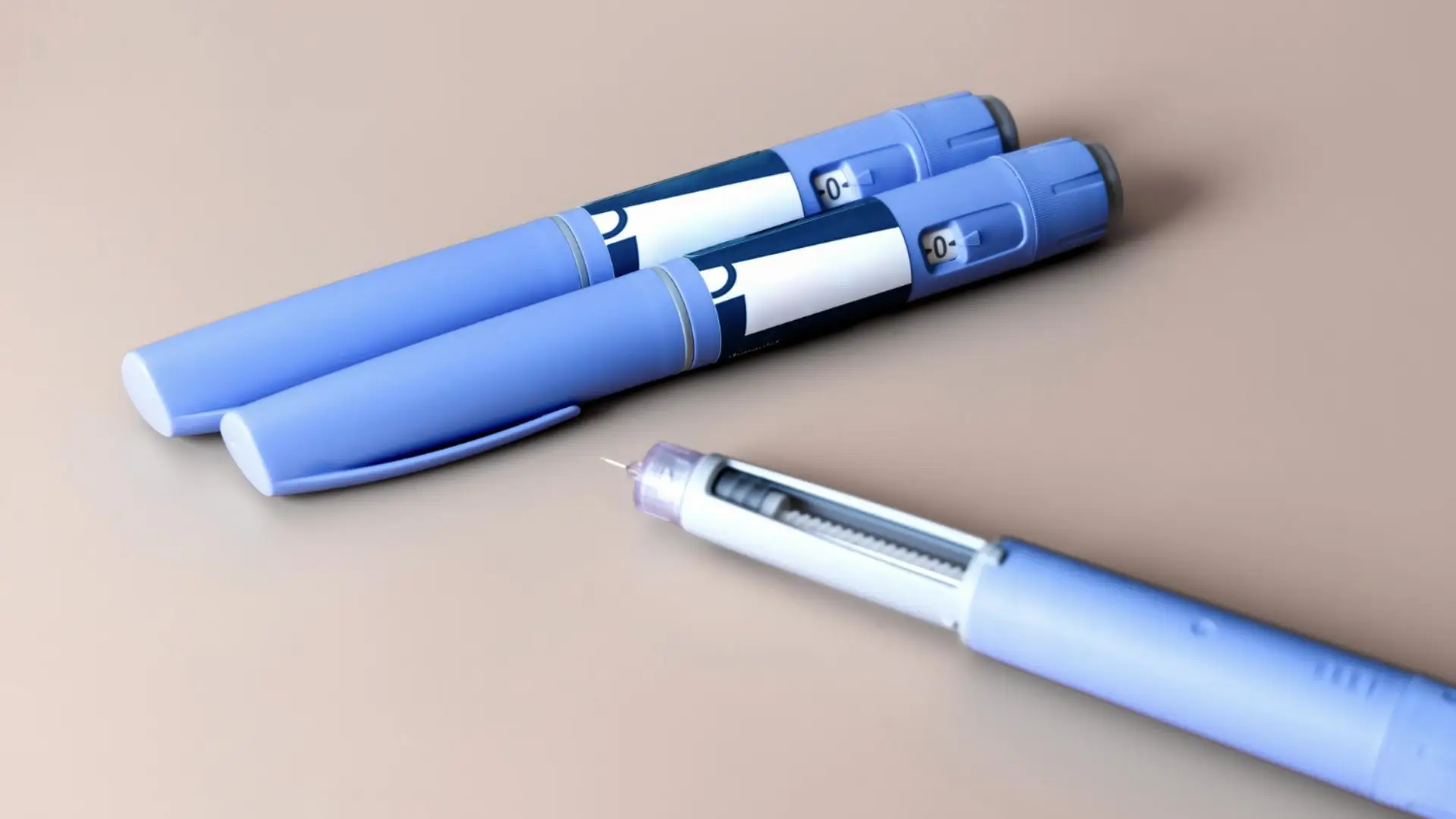
A balanced diet is one of the most effective ways to manage type 2 diabetes, especially when paired with medications like Ozempic (semaglutide). The American Diabetes Association notes that smart nutrition supports blood sugar control, heart health, and weight management, complementing medical therapy.
For those using Ozempic, maintaining healthy eating habits can do more than boost results—it can also make the treatment easier to tolerate. While Ozempic doesn’t have any strict food restrictions or direct drug–food interactions, certain foods may intensify gastrointestinal side effects such as nausea or bloating. Learning which foods to avoid and which to prioritize can help patients feel more comfortable and stay on track with their therapy.
In this article, we’ll explore which foods to avoid while taking Ozempic, why some may worsen side effects, and how to build a sustainable, diabetes-friendly diet that supports both metabolic health and overall well-being.
Key Takeaways
- Ozempic (semaglutide) helps manage type 2 diabetes and supports weight loss, but certain foods can make side effects worse.
- High-fat, fried, and sugary foods slow digestion, intensify gastrointestinal symptoms, and may interfere with treatment comfort and adherence.
- Ozempic has no major food–drug interactions. However, patients may benefit from tailored dietary guidance to complement the medication’s effects on digestion.
- A balanced diet rich in lean proteins, whole grains, and non-starchy vegetables promotes smoother digestion and steadier blood sugar levels.
- Hydration is critical. Drink enough water and limit alcohol or caffeine, which can worsen dehydration and nausea.
- Keeping a food and symptom journal helps identify individual triggers and allows clinicians to fine-tune meal plans and Ozempic dosage adjustments.
- Ongoing communication with healthcare professionals and dietitians ensures patients safely manage side effects and achieve the best possible long-term outcomes.
About: Medica Depot is your trusted all-in-one supplier, offering a range of high-quality medical injectables and supplies. If you’re looking to buy Ozempic, contact Medica Depot’s sales representatives and they will guide you on how to do so. Whether for health professionals, plastic surgeons, dermatologists, licensed estheticians, or other specialists, we can offer genuine, brand-name products you may need. With Medica Depot, we prioritize serving you better to improve the patient’s quality of life.
Why Certain Foods Worsen Ozempic Side Effects
For individuals taking Ozempic, mindful eating plays an essential role in promoting health and comfort during treatment. While the medication is highly effective in improving glycemic control and supporting weight management, certain foods may intensify side effects and make the experience less tolerable. Understanding which specific foods to limit or avoid can reduce uncomfortable side effects and improve adherence to therapy.
Healthcare professionals often recommend personalized dietary guidance for people managing type 2 diabetes. Even when taking Ozempic (semaglutide), maintaining mindful eating habits is essential to ensure comfort, support treatment goals, and minimize side effects.
While Ozempic has no significant food–drug interactions, certain foods can aggravate gastrointestinal symptoms or contribute to long-term discomfort if not properly managed. Understanding these triggers helps patients reduce both short-term and long-term side effects of Ozempic.
Ozempic works as a GLP-1 receptor agonist, slowing gastric emptying and increasing satiety so that food stays in the stomach longer. Because of this, nutrition counseling plays a key role in improving tolerance and adherence. Registered dietitians often guide patients to avoid greasy, heavy meals and high-sugar drinks during treatment, reintroducing a broader range of foods gradually as the body’s health adjusts.
Common Triggers: High-Fat, Fried, and Sugary Foods With Ozempic

An Ozempic-friendly diet helps improve blood sugar control, support weight loss, and reduce side effects. Choosing smaller, lighter meals and focusing on nutrient-dense, easily digestible foods can make a noticeable difference in how patients feel during treatment.
Patients should avoid foods that can trigger or increase side effects while taking Ozempic. Meals that are high in fat or difficult to digest can lead to persistent gastrointestinal distress, especially on an empty stomach.
Some of the most common trigger foods include:
- Greasy and Fatty Meals: High-fat foods delay digestion even further, amplifying Ozempic’s gastric-retention effect. This can increase side effects, such as nausea, bloating, reflux, and vomiting. Limiting these foods can significantly improve comfort and tolerability.
- Sugary Foods and Refined Carbohydrates: Sweets, pastries, and sugary drinks can cause blood sugar spikes and worsen gastrointestinal upset. They also add unnecessary calories that work against weight-loss goals.
- Fried Chicken and Heavily Processed Foods: These foods combine high fat and low digestibility, increasing the risk of persistent GI discomfort, especially during dose titration or adjustment phases.
- Dairy Products: Full-fat milk, cheese, and cream may slow digestion and exacerbate nausea, particularly when taken on an empty stomach. Patients sensitive to dairy products should limit their intake until their body adjusts.
These specific foods do not directly interact with the drug, but their composition can magnify side effects associated with delayed gastric emptying. Patients who avoid foods high in fat and sugar typically report fewer uncomfortable side symptoms.
Best Dietary Practices for Patients Using Ozempic

To ensure a safe and effective Ozempic journey, patients should work closely with healthcare providers who can provide individualized advice on Ozempic dosage, administration, and diet.
- Choose lean proteins such as fish, poultry, tofu, and legumes to maintain muscle mass and support steady blood sugar levels.
- Incorporate whole grains, non-starchy vegetables, and fiber to improve digestion and reduce bloating.
- Stay hydrated throughout the day, and limit alcohol and caffeine, both of which can worsen dehydration and nausea.
Keeping a food and symptom journal helps patients identify personal triggers, monitor side effects, and share useful observations with their dietitian or physician. Persistent or worsening symptoms should always be discussed with a healthcare professional to prevent complications.
Clinician Guidance for Counseling on Ozempic and Nutrition

The U.S. Food and Drug Administration (FDA) has approved Ozempic for adults with type 2 diabetes to:
- Improve blood sugar control when combined with diet and exercise.
- Reduce the risk of major cardiovascular events in those with established heart disease.
- Decrease the risk of kidney disease progression in patients with type 2 diabetes and chronic kidney disease.
To help patients manage side effects, clinicians may recommend:
- Eating bland foods and adding ginger to ease mild nausea.
- Taking short walks after meals to aid digestion.
- Promptly reporting persistent or severe symptoms such as vomiting, dehydration, or abdominal pain for evaluation and management.
Healthcare providers should also reinforce proper injection technique, titration schedules, and follow-up visits to optimize treatment outcomes.
Conclusion on the Best Foods For Health On Ozempic Treatment
Managing food intake while on Ozempic is key to achieving better results and avoiding unnecessary discomfort. By limiting greasy, sugary, and highly processed foods, patients can reduce side effects and support long-term success.
Emphasizing balanced meals with lean proteins, whole grains, and vegetables can help stabilize blood sugar, enhance energy, and complement Ozempic’s effects. Continuous communication with healthcare providers ensures safe adjustments and empowers patients to maintain a sustainable, healthy eating pattern throughout treatment.
FAQs
1. What foods should patients avoid while taking Ozempic?
While taking Ozempic, it’s best to avoid greasy and fatty meals, sugary drinks, refined carbohydrates, fried foods, and heavily processed items. These foods can worsen side effects such as nausea and bloating, while also affecting glycemic control.
2. How does a diet impact the effectiveness of Ozempic?
A balanced diet enhances the effectiveness of Ozempic. Foods that are low in fat and sugar can improve tolerability. This helps in managing blood sugar levels and supports the weight-loss goals that often accompany Ozempic treatment.
3. What dietary practices should patients follow while using Ozempic?
Focus on lean proteins, whole grains, and non-starchy vegetables. Stay hydrated and limit alcohol and excessive caffeine. Keeping a food and symptom journal can help identify personal triggers and improve dietary habits for better outcomes.
References
American Diabetes Association. Tips for Eating Well | Eat Good to Feel Good. diabetes.org. Published 2024. Accessed October 8, 2025. https://diabetes.org/food-nutrition/eating-healthy
Cleveland Clinic. Can Certain Foods Impact Your Ozempic Side Effects? Cleveland Clinic. Published August 5, 2024. Accessed October 8, 2025. https://health.clevelandclinic.org/ozempic-foods-to-avoid