For many people, the thought of needles or minor procedures can be unsettling. Fortunately, topical anesthetic creams like those containing lidocaine can help take the edge off. Studies show that applying a numbing cream before procedures like intravenous cannulation can significantly reduce pain and discomfort, making medical experiences more manageable.
One widely used option is Emla Cream, a topical anesthetic that combines lidocaine and prilocaine to create a localized numbing effect or sensation. Whether for medical treatments or cosmetic procedures, its ability to minimize pain makes it a popular choice among healthcare professionals.
But how long does Emla Cream actually last? In this article, we’ll break down how long its effects last, how to use it properly, what factors influence its effectiveness, and any potential side effect to be aware of.
Key Takeaways
- Emla Cream combines 2.5% lidocaine and 2.5% prilocaine to relieve localized pain for medical and cosmetic procedures.
- The onset of Emla Cream’s effects generally takes one hour on intact skin and 5 to 10 minutes on genital mucous membranes.
- Maximum analgesia is achieved 2 to 3 hours after application and lasts 1 to 2 hours on intact skin once removed.
- Factors like skin condition, application technique, and patient age can influence the cream’s effectiveness and absorption.
- Prolonged use carries risks such as systemic toxicity and local skin reactions, making correct application essential for safety.
About: Medica Depot is your trusted all-in-one supplier, offering a range of high-quality medical injectables and supplies. Our sales representatives can advise you on how to Buy Emla online today! Whether for health professionals, plastic surgeons, dermatologists, licensed estheticians, or other specialists, we can offer genuine, brand-name products you may need. With Medica Depot, we prioritize serving you better to improve the patient’s quality of life.
Onset and Duration of Emla Cream’s Anesthetic Effects
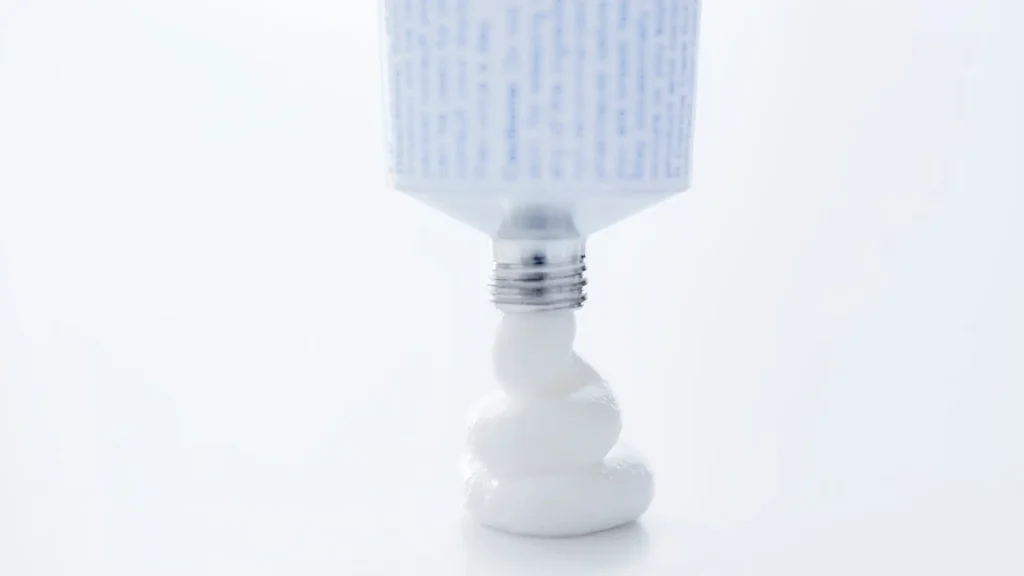
Emla Cream’s generic name, lidocaine-prilocaine, reflects its two active ingredients, which are widely recognized for their safety and efficacy in providing dermal analgesia when applied to intact skin. The U.S. Food and Drug Administration (FDA) has approved this topical anesthetic for use on normal, intact skin and genital mucous membranes.
Each tube of Emla Cream contains a eutectic mixture of 2.5% lidocaine and 2.5% prilocaine. These anesthetics stabilize neuronal membranes by blocking the ionic fluxes required for initiating and transmitting nerve impulses, effectively numbing the area.
Onset, Maximum Effect, and Duration
The onset, depth, and duration of Emla Cream’s anesthetic effect depend on application time:
- Onset: 1 hour on intact skin; 5 to 10 minutes on genital mucous membranes.
- Maximum Effect: Reached 2 to 3 hours after application.
- Duration: Lasts 1 to 2 hours after removal on intact skin; 15 to 20 minutes on genital mucous membranes.
For procedures like intravenous catheter placement or venipuncture, apply Emla Cream under an occlusive dressing with an application time of at least one hour to ensure adequate pain relief.
Factors That Influence Effectiveness and Absorption Time

Medical professionals should discuss the factors influencing Emla Cream’s effectiveness, helping patients make informed treatment decisions. Several variables, including skin condition, application technique, and individual patient characteristics, can impact its absorption and efficacy.
- Application Technique: Proper application is essential for maximum effectiveness. Practitioners should be trained in applying topical anesthetic creams correctly, including the use of an occlusive dressing, which significantly enhances absorption.
- Dosage and Duration: Following the recommended amount and application time ensures optimal dermal analgesia. Deviating from guidelines may lead to reduced effectiveness.
- Patient Age and Skin Health: Younger patients and those with healthy skin tend to absorb the cream more quickly, experiencing more effective anesthesia. In contrast, older individuals or those with compromised skin integrity may have slower absorption and less pronounced effect.
Comparison with Other Topical Anesthetics
The FDA approval of Emla Cream has led to its widespread use among medical professionals for procedures requiring dermal analgesia. Studies have shown its superior effectiveness in pain reduction compared to other topical anesthetics.
A comparative study found that both Emla Cream and ELA-Max provided better pain relief than tetracaine gel and betacaine-LA, particularly after a 60-minute application and even within 30 minutes. All topical anesthetics in the study demonstrated increased clinical efficacy 30 minutes after removal, but Emla Cream consistently delivered stronger pain relief.
Another study compared Emla Cream with lidocaine tape for venipuncture pain. The findings indicated that Emla Cream provided significantly better pain relief, making it the preferred choice for minimizing discomfort during venipuncture.
Safety Concerns and Potential Risks of Prolonged Use

Before using Emla Cream, patients should consult their doctor to determine its suitability and fully understand the risks and benefits of this anesthetic solution. Prolonged or excessive use of Emla Cream, which contains lidocaine and prilocaine, may lead to serious safety concerns, including systemic toxicity if applied over large areas or for extended periods.
A systematic review found that systemic toxicity can cause severe complications, such as methemoglobinemia, central nervous system toxicity, and cardiotoxicity. Methemoglobinemia, in particular, presents as brownish cyanosis that does not improve with oxygen administration and can be life-threatening if not treated promptly.
Potential Side Effects of Emla Cream
- Local Skin Reactions: Common side effects include erythema, edema, and abnormal sensations at the application site. These reactions are usually mild but can become more severe with prolonged use.
- Allergic Reactions: Hypersensitivity to lidocaine, prilocaine, or other components of the cream can lead to severe allergic reactions, such as hives, difficulty breathing, and swelling of the face, lips, or throat.
- Increased Absorption: Some may ask, “Can you put Emla Cream on a burn?” It’s worth noting that applying the cream to broken or inflamed skin can enhance systemic absorption, increasing the risk of toxicity.
Conclusion
Emla Cream is a trusted topical anesthetic that effectively relieves pain during various medical and cosmetic procedures. It numbs the application area by combining lidocaine and prilocaine, ensuring greater patient comfort during treatments. The onset and duration of its effects depend on factors such as the application site and individual skin characteristics.
While Emla Cream is highly effective, it is essential to use it correctly and be aware of potential risks like systemic toxicity and local skin reactions, especially with prolonged or excessive application. Consulting a medical doctor ensures safe and proper use, allowing patients to benefit from its analgesic properties while minimizing risks.
FAQs
1. How long does it take for Emla Cream to start working?
Emla numbing cream typically takes effect within one hour when applied to intact skin. However, on genital mucous membranes, it can work in just 5 to 10 minutes.
2. How long do the effects of Emla Cream last after application?
The analgesic effects of Emla Cream last for about 1 to 2 hours after removal from intact skin, while on genital mucous membranes, the effects last around 15 to 20 minutes.
3. What factors can influence the effectiveness of Emla Cream?
The effectiveness of Emla Cream can be influenced by skin thickness, the application technique, the amount of cream used, and the age and health of the patient. Proper application under an occlusive dressing enhances absorption and effectiveness.
References
- Ramaiah, P., Elsayed, L. A., & Khamis, H. M. A. (2015). Efficacy of Topical Anesthesia Cream in Reducing the Pain Associated with Intravenous Cannulation. International Journal of Science and Research (IJSR) ISSN, 5, 2319–7064. https://doi.org/10.21275/ART20163785
- Friedman, P. M., Fogelman, J. P., Nouri, K., Levine, V. J., & Ashinoff, R. (1999). Comparative Study of the Efficacy of Four Topical Anesthetics. Dermatologic Surgery, 25(12), 950–954. https://doi.org/10.1046/j.1524-4725.1999.99138.x









